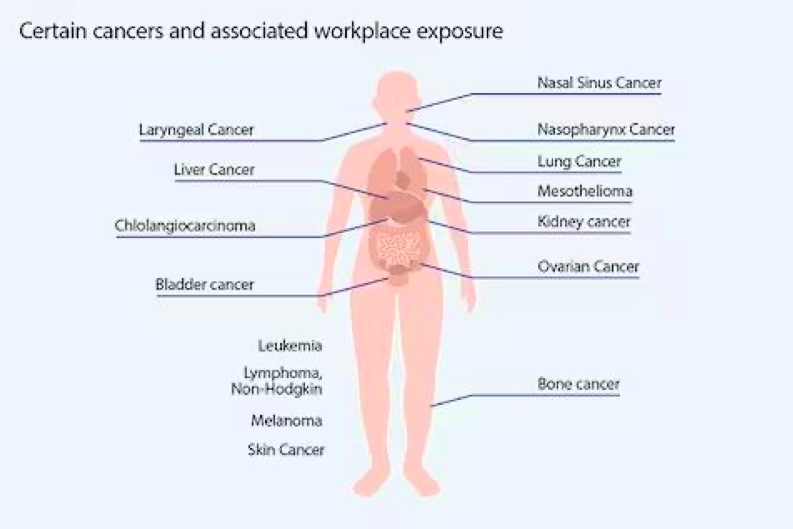
As with a vast number of aspects of medicine, an understanding of the pathophysiology and risk factors of diseases are still being understood. Evidence has shown a correlation between certain workplace-associated factors and an increased risk of cancer. The implications of exposure to chemicals and other risk factors continue to be seen in higher proportions within the cancer patient cohort, most notably from significant asbestos exposure and its link with mesothelioma.
Certain types of work carry a slightly higher risk. This is dependent on what workers are exposed to, as well as the frequency and intensity of said exposure.
Types of work that could carry a higher risk include:
Occupational cancers are those that occur due to exposure to carcinogenic agents in the workplace. Exposures include:
- A wide range of different chemicals, dusts, metals and combustion products (e.g. asbestos or diesel engine exhaust)
- Forms of radiation (e.g UV or ionising radiation)
- Exposures to metals
- Patterns of behaviours (e.g. shift working)
- Handling of cytotoxic chemicals/drugs
Risks in healthcare
As healthcare professionals, there are cancer risks within the workplace. For cancer nurses, the most obvious culprit of this is due to handling cytotoxic drugs. An increased risk is seen both during administration and handling of the product, as well as handling waste products, including urine, of patients after they’ve received cytotoxics.
Exposure and risk is also increased through exposure to radiation, including whilst care for patients receiving radio-iodine for thyroid cancer or following PET scan where a radioactive dye is used.
Is it crucial that handling of these drugs, and care of these patients is only undertaken by staff who have been suitably trained, and with the use of appropriate PPE and implementation of safety precautions. Whilst planning pregnancy, during pregnancy or whilst breastfeeding, particular care is necessary to protect both mother and baby. Where possible, preference should be for avoiding these risk factors completely, especially during the first trimester.
How have things changed?
In 2015, exposure to health hazards at work were thought to have caused 9,000 cases of cancer in the UK (Cancer Research, 2020). Importantly, many of these cases were due to exposures from a long time ago when health and safety rules were less developed. However, according to the Roadmap on Carcinogens (2016), approximately 120,000 work- related cancer cases occur each year as a result of exposure to carcinogens at work in the EU, with approximately 80,000 fatalities annually.
Thankfully, these significant and alarming statistics prompted change in law and workplace health and safety measures to reduce the exposure and associated risk of workplace related cancer.
Employers have a legal duty to protect the health and safety of their employees, through prevention or limitation of exposure to cancer-causing substances.
In 2017, the European Commission committed to protecting workers from work-related cancer through an initiative on safety and health at work.
This endeavoured to:
- Set exposure limits or other measures (e.g.
suitable PPE) for seven cancer-causing substances. There are strict labour laws that limit exposure to harmful chemicals and other hazards at work. - Help businesses in their efforts to comply with
health and safety rules. - Reduce the focus on paperwork and simplify administrative burden while
maintaining worker protection.

Reducing exposure
There are a number of actions workers can take to limit their exposure and risk of workplace-related cancer.
- Avoid asbestos - it is not usually possible to identify asbestos without training. If there is any concern of asbestos, seek advice from an approved contractor or specialist in asbestos management.
- Work safely in the sun - spend time in the shade, wear a hat, use suncream.
- Use effective PPE and/or limit time and exposure to chemicals, cytotoxics. Ensure
regular and up-to-date training in the safe management of these substances.
Psychological implications of workplace-related cancer diagnosis
The social and emotional impact of a cancer diagnosis is well documented. It is estimated that 70% of cancer survivors experience depression at some point (MD Anderson Cancer Centre, 2023).
Supporting patients to come to terms with a ‘workplace-related’ cancer diagnosis can be difficult in a very different way. Feelings of injustice, frustration and grief are common and helping a patient adjust to a cancer diagnosis when ‘they have done nothing wrong’ can be incredibly difficult. Often, those who stick in the memory are the ones with lung cancer associated with asbestos when they ‘have never smoked’. There is a real feeling of unfairness and frustration.
As with any cancer diagnosis, whether risk driven or misfortune, allowing them to vent, to find coping mechanisms and methods of processing such a difficult time in their lives are often the most beneficial things we can do as healthcare professionals to support them.
What can we do?

Rates of cancers related to workplace risks and exposures remain common within cancer care settings.
● Changes in practice,
● Awareness of the risks
● Appropriate and regular training
These will all contribute to reducing this prevalence and making the workplace a safer place.
We must also:
★ Support others
★ Raise awareness of risk factors with friends/family/colleagues
Take care of yourselves.